Your co-workers throughout the UConn Health community ask you to join them in raising breast cancer awareness by wearing pink on Friday. Shout out to the UConn Health Internal Medicine sites in East and West Hartford for participating in the cancer center’s Community Breast Navigation Program this year! With their help and expertise, the grant funded outreach program was able to educate women on the importance of screening and provide seamless navigation to screening.
Patient Care
Looking at Us: In Compliance With Deb Abromaitis

One of the reasons for the UConn John Dempsey Hospital’s high marks in the latest Joint Commission survey is the work of the Office of Healthcare and Regulatory Compliance. Longtime UConn Health nurse and nurse administrator Deb Abromaitis serves as its interim compliance officer, and she credits her staff (and many others) for the successful visit. Today we get to know Deb a little better. She lives in Unionville with her husband, and has two grown sons and two grandchildren.

Deb Abromaitis
Favorite sport:
Figure skating
Favorite holiday:
Christmas. I love giving puzzles to my nieces, nephews and my children to figure out how to solve the puzzle to get a gift.
Favorite place(s) to visit:
Istanbul, Turkey. I also love to vacation in the Outer Banks with friends.
Favorite dining spot:
I love going out to different restaurants for breakfast on the weekend with my husband and friends.
Interest outside of work:
I always love and treasure spending time with my family.
Describe your role here, and how your roles have changed/evolved over the years?
I’ve been the Interim Compliance Officer in the Office of Healthcare and Regulatory Compliance for less than a year. The first time I worked at UConn Health was about 30 years ago, and I have been in many positions over the years, starting as a per diem nurse then a nursing supervisor, manager, and director.
Some of the areas where I have managed include the Nursing Supervisors, Bed Control, Float Pool, Transportation, Emergency Management, Environment of Care, Patient Relations, Volunteers, Spiritual Services, Interpreters, Quality and Regulatory.
When you were first starting as a nurse, if someone told you that you’d be a hospital compliance officer, how would you have reacted?
I would never have believed it! I love people and knew that as long as I was a nurse I would never be anywhere but at the bedside!
What are the most challenging and rewarding aspects of your job today?
The most challenging would be having others understand that we are trying to be helpful when we work with areas to meet the needs and regulatory requirements for the patients, the staff and the institution.
The most rewarding is watching patient care improve, staff pride and satisfaction grow, and the institution get recognized for the great work that we do and the care that we provide.
We recently had an unannounced accreditation survey by The Joint Commission. What goes into preparing for and dealing with that, and what made it successful?
In the hospital we say that we are always prepared for a survey. It’s working hard every day to do everything possible to educate and train all staff to meet all regulations to provide the highest level of care to all patients.
What made it successful is the commitment of everyone at UConn Health to remain regulatory compliant and provide the highest level of care to our patients. We hear that it takes a village….and it truly does! There are so many employees who work very hard and are willing to do whatever they can to help have a positive impact on our survey. They are sincerely appreciated!
I don’t want to name individuals as I know I would feel terrible about leaving out the many, many people who were instrumental in this success. I do need to recognize Dr. Agwunobi’s constant support of the readiness process, including his commitment to securing repeated visits from The Joint Commission Resource consultants who helped us prepare for the actual survey. In addition, I do need to highlight:
- My staff in the Office of Healthcare and Regulatory Compliance, who worked tirelessly for months training and obtaining all documents needed.
- Senior leadership, who provided a plethora of time and support as well as vision.
- Chapter leaders, who ensured compliance and readiness with Joint Commission standards.
- Nursing and all staff who worked tirelessly to prepare their units and the entire hospital to be ready for the survey each day. Those who willingly spoke with Joint Commission surveyors and shared the positive aspects of what we do were terrific!
- Support staff who assisted day in and day out as ambassadors, scribes, runners, drivers, catering, maintenance, facilities, housekeeping.
Everyone worked together to ensure we showed The Joint Commission the best of UConn John Demspey Hospital. The work of so many wonderful, dedicated staff made the entire survey an incredible success!
And when you’re not working, you’re often volunteering?
I love to volunteer, including being the opening ceremonies and figure skating competitions director and coordinator for the Connecticut Special Olympics for many years, volunteering on the Community Emergency Response Team (CERT), fundraising for the American Heart Association, and I’m very proud that I brought and chaired the first Relay for Life in Farmington!
Your family seems to have several connections with UConn basketball.
My husband played basketball at UConn (Jim Abromaitis, 1975-1980). My older son played basketball at Yale (Jason Abromaitis, 2003-2007), and married Ann Strother, who played basketball at UConn. They have two children, a 3-year-old boy and 1-year-old girl. My other son played basketball at Notre Dame (Tim Abromaitis, 2007-2012). I never played basketball, but was a UConn cheerleader.
UConn Health October 2018 Programs, Events
 Here is a list of UConn Health programs scheduled for October and early November 2018. This information will be updated with any additions or other schedule changes. (Last updated 10/15)
Here is a list of UConn Health programs scheduled for October and early November 2018. This information will be updated with any additions or other schedule changes. (Last updated 10/15)
Living Well With Epilepsy: A Support Group for Young Adults
Saturday, Oct. 6, noon to 1:30 p.m., UConn Health Outpatient Pavilion, 2nd floor large conference room S2010
The Epilepsy Foundation of Connecticut, in partnership with the UConn Health Department of Neurology, offers a support group for young adults who live with epilepsy. This group is open to those aged 18 to 30 who would like to join others to share experience, gain peer support, and learn together about epilepsy and overcoming its challenges to live well. The group generally meets on the first Saturday of the month. Please call 860-346-1924 or email manzelone.efct@sbcglobal.net for more information.
Bladder Cancer Support Group
Saturday, Oct. 6, 2 to 3 p.m., UConn Health, Onyiuke Dining Room
Patients, family members and caregivers (not limited to UConn Health patients) are invited to join others whose lives have been touched by bladder cancer. This month, UConn Health’s oncology dietitian joins as a guest speaker. This support group, established in partnership with the Bladder Cancer Advocacy Network, usually meets on the first Saturday of the month and is the only group of its kind in New England. Call 888-901-BCAN for more information.
Free Hospital Maternity Tours
Saturday, Oct. 6, 2 p.m., UConn Health, University Tower lobby
A representative will guide you through labor and delivery, postpartum, and the nursery at the UConn John Dempsey Hospital. Children and grandparents are welcome. Call 800-535-6232 to register or for more information.
Breastfeeding Class
Wednesday, Oct. 10, 6 to 8 p.m., UConn Health Outpatient Pavilion, 3rd floor large conference room S3301
A certified lactation consultant leads a discussion of topics including the benefits of breastfeeding, how to get started, and how the rest of the family can help the breastfeeding mother as well as how to continue breastfeeding and working. Fee is $25 per couple. Call 800-535-6232 to register or for more information.
Childbirth Preparation Class
Wednesday, Oct. 17, 6 to 10 p.m., UConn Health Outpatient Pavilion, 3rd floor large conference room S3301
This one-day class covers anatomy and physiology of pregnancy and labor, emotions of pregnancy, nutrition, fetal growth and development, comfort measures for labor, working with unexpected events in labor, cesarean delivery, and practice of relaxation and breathing techniques for labor. Class size is limited to eight couples. Remember to bring two pillows and wear comfortable clothing. Light snack is provided. Fee is $100. Call 800-535-6232 or 860-679-7692 to register or for more information.
(Corrected 10/15)
Living With Heart Disease Meeting
Thursday, Oct. 18, 11 a.m. to noon, UConn Health, University Tower, 2nd floor conference room
Men and women affected by heart disease meet on the third Thursday of every other month to discuss post-diagnosis topics such as prevention and wellness, social and emotional support, heart-healthy recipes, coping strategies and resources. Significant others and caregivers are also welcome to attend. Please call Sue at 860-679-3633 for more information.
Breast Cancer Support Group
Thursday, Oct. 18, 7 to 8 p.m., UConn Health, Onyiuke Dining Room
This is a support group intended for women under the age of 45 who’ve been diagnosed with non-metastatic breast cancer. Women at any point in their cancer survivorship journey are welcome. Meetings are the third Thursday of the month. To register or more information, call 860-679-7820 or email tillinghast@uchc.edu.
Infertility Peer Support Group
Thursday, Oct. 18, 7 to 8:30 p.m., Center for Advanced Reproductive Services, 2 Batterson Park Road, Farmington.
The Greater Hartford chapter of RESOLVE, a national nonprofit resource for those facing the challenges of infertility, offers support, information and confidential, informal, peer-led discussions on the third Thursday of the month. To learn more or to check for weather-related cancellation, call 860-523-8337.
Free Hospital Maternity Tours
Saturday, Oct. 20, 2 p.m., UConn Health, University Tower lobby
A representative will guide you through labor and delivery, postpartum, and the nursery at the UConn John Dempsey Hospital. Children and grandparents are welcome. Call 800-535-6232 to register or for more information.
Free Cosmetology Services for Cancer Survivors
Monday, Oct. 22, 1 to 3 p.m., UConn Health Outpatient Pavilion, 4th floor
“Look Good…Feel Better” is a free program to help improve the self-image and self-esteem of women experiencing appearance-related side effects from cancer treatment. During this hands-on workshop, a trained volunteer certified cosmetologist will teach women how to cope with skin changes and hair loss using cosmetic and skin care products donated by the cosmetic industry. Classes are offered every other month and are not limited to UConn Health patients. Please call 860-679-7820 to register (required).
Stroke Survivor Group
Wednesday, Oct. 24, noon to 1 p.m., UConn Health Outpatient Pavilion, 3rd floor
The UConn Health Stroke Center invites stroke survivors, families and caregivers to a monthly group meeting to discuss topics such as prevention, coping methods, support systems, rehabilitation tips, resources, and promoting independence. The Stroke Survivor Group generally meets on the fourth Wednesday of the month. Call 860-679-4846 for more information.
Free Workshop: “Things to Consider Before Joining a Research Study”
Monday, Oct. 29, 5 p.m., UConn Health, Onyiuke Dining Room
The UConn Health Human Subjects Protection Office offers an educational session about the rights and responsibilities of participants in research projects on the last Monday of the month. Registration is required: 860-679-8802 or cagganello@uchc.edu.
Living Well With Epilepsy: A Support Group for Young Adults
Saturday, Nov. 3, noon to 1:30 p.m., UConn Health Outpatient Pavilion, 2nd floor large conference room S2010
The Epilepsy Foundation of Connecticut, in partnership with the UConn Health Department of Neurology, offers a support group for young adults who live with epilepsy. This group is open to those aged 18 to 30 who would like to join others to share experience, gain peer support, and learn together about epilepsy and overcoming its challenges to live well. The group generally meets on the first Saturday of the month. Please call 860-346-1924 or email manzelone.efct@sbcglobal.net for more information.
Bladder Cancer Support Group
Saturday, Nov. 3, 2 to 3 p.m., UConn Health, Onyiuke Dining Room
Patients, family members and caregivers (not limited to UConn Health patients) are invited to join others whose lives have been touched by bladder cancer. This support group, established in partnership with the Bladder Cancer Advocacy Network, usually meets on the first Saturday of the month and is the only group of its kind in New England. Call 888-901-BCAN for more information.
Free Hospital Maternity Tours
Saturday, Nov. 3, 2 p.m., UConn Health, University Tower lobby
A representative will guide you through labor and delivery, postpartum, and the nursery at the UConn John Dempsey Hospital. Children and grandparents are welcome. Call 800-535-6232 to register or for more information.
Breastfeeding Class
Wednesday, Nov. 14, 6 to 8 p.m., UConn Health Outpatient Pavilion, 3rd floor large conference room S3301
A certified lactation consultant leads a discussion of topics including the benefits of breastfeeding, how to get started, and how the rest of the family can help the breastfeeding mother as well as how to continue breastfeeding and working. Fee is $25 per couple. Call 800-535-6232 to register or for more information.
(Corrected 10/15)
Living With Heart Disease Meeting
Thursday, Nov. 15, 11 a.m. to noon, UConn Health, University Tower, 2nd floor conference room
Men and women affected by heart disease meet on the third Thursday of every other month to discuss post-diagnosis topics such as prevention and wellness, social and emotional support, heart-healthy recipes, coping strategies and resources. Significant others and caregivers are also welcome to attend. Please call Sue at 860-679-3633 for more information.
Free Hospital Maternity Tours
Saturday, Nov. 17, 2 p.m., UConn Health, University Tower lobby
A representative will guide you through labor and delivery, postpartum, and the nursery at the UConn John Dempsey Hospital. Children and grandparents are welcome. Call 800-535-6232 to register or for more information.
Directions to UConn Health are available at health.uconn.edu/locations.
Looking at Us: Ellen ‘Bleeds Blue’ Benson, OR Nurse Manager
More than 11,000 surgeries are performed here every year from foot surgery to brain surgery which takes a lot of coordination and planning to make sure patients get the best care possible. A key reason our ORs run smoothly and efficiently is the dedication and tireless work of nurse manager Ellen Benson. She’s worked at UConn Health for the last 28 years. Ellen lives in Harwinton with her husband of 36 years. She has three grown children.
 Ellen Benson
Ellen Benson
Favorite book:
I was never much of a reader, but I fell in love with Edgar Allan Poe when I was a kid, weird little short stories, they were great for my attention span at the time
Favorite movie:
I love Harry Potter and Indiana Jones movies.
Favorite time of year:
I love the fall. The cool crisp air, the colors, the smells and the comfort foods (like apple crisp and ice cream). Halloween is one of my favorite “holidays.”
Favorite place to visit:
This is a toss- up. I love the beach and I also love to hike in the woods, no particular location. As long as my family is with me, I’m happy anywhere.
Famous person you’d most like to meet:
Colin Powell. I read his autobiography and was amazed at his life story, the places he has traveled, the work he did, the people that he knew. I would also have loved to have met and worked with Florence Nightingale – she is my hero!
Something about you today that your younger self would never believe:
That I would love my job even more today than I did when I first started and that I would be the manager of the OR.
Why did you become a nurse?
I went to a career fair when I was 18 years old and was introduced to the surgical technology profession. I grew up butchering chickens with my grandfather, so I thought – I can do that job! I worked for about a year full time and then realized I could do more, so my husband encouraged me to go to nursing school.
How did you end up being the OR nurse manager?
I worked for nearly 19 years from 3 to 11 p.m. as a staff nurse. That was an extraordinary opportunity because I learned so much. I worked with a small group who really helped each other and it was an awesome environment. Working evenings also gave me the opportunity to be home during the day with my children. It was the perfect work/life balance for us. When my youngest daughter was in high school, my husband said it was time to switch shifts. It just so happened that the assistant nurse manager position opened up. I had never thought about going into management but I thought that it might be a good move for me. I got the position and learned many new skills. When the manager position became available, a few people encouraged me to apply. Much to my surprise, I was hired for the position and have been the manager for almost five years now.
What has been a major milestone in your career?
I earned my bachelor’s degree about a year ago. That was a huge personal achievement! I was highly encouraged to complete my degree by nursing administration and they really supported me through the process. I enjoyed taking classes with the younger students who were fresh out of their associate degree programs. I have worked in the OR my whole life so it was great looking at nursing through their eyes. I ended up being a mentor to quite a few of them and I still stay in touch with them, so that was really a wonderful experience. My husband and children also helped me achieve this milestone, if it weren’t for their support, it would have never happened.
Why do you like working at UConn Health?
It’s just a wonderful place to work. We have this beautiful new hospital and we have great nurses, physicians and support staff to help us fulfill our mission of teaching and caring for the people of the state of Connecticut.
I love coming to work every day. I am proud to be a part of the UConn family.
I really do bleed blue!
Spotlight on Services: Sports Cardiology

Sports cardiology is an emerging subspecialty with a focus on highly active people. It’s now available at the Pat and Jim Calhoun Cardiology Center, where Drs. Kai Chen and Peter Schulman are among those trained in this discipline, supporting not only UConn athletics but also the Connecticut Sun professional women’s basketball team and the New England Black Wolves professional lacrosse team.
What is sports cardiology?
Chen: Sports cardiology is cardiology related to sports and exercise, an entity incorporating all ages, from childhood to the senior population, and all forms of exercise activity, including professional, recreational, and occupational. Starting with the care of competitive athletes, sports cardiology has expanded to include the general population in the prevention and management of cardiac conditions during exercise.
Who is a candidate to see a sports cardiologist?
Chen: Sports cardiology takes care of athletes and anyone who exercises. Candidates for a sports cardiology evaluation include:
- Healthy people with a family history of cardiac condition before participation in sports or exercise.
- Anyone with new symptoms during exercise or sports participation such as lightheadedness, palpitation, shortness of breath, chest discomfort, or unexplained drop in exercise tolerance.
- Patients with known cardiovascular disease who want to return to exercise and stay active.
How does this discipline fit in with the service as team physicians to the UConn athletic programs?
Schulman: UConn Health physicians serve as the team physicians for UConn athletes, and this is part of sports cardiology. For example, we screen the UConn athletes as they prepare for the upcoming season. Sports injuries and other medical conditions are handled by the UConn infirmary and UConn Health providers in Storrs. Between these two services, UConn athletes have all of their health needs served.
What’s the difference between athletic heart syndrome and hypertrophic cardiomyopathy?

Schulman: Due to increased metabolic demands of athletic performance, the athlete’s heart adapts to the enhanced metabolic needs by undergoing structural changes to increase the ability of the heart to pump blood. These changes include “bulking up” or hypertrophy of the heart muscle and increasing the size of the heart chambers to handle the increased blood flow. These changes are part of the “athletic heart syndrome.” On the other hand, there are some diseases of the heart muscle such as hypertrophic cardiomyopathy (HCM) that can cause adverse structural changes of the heart. HCM can appear superficially similar to the normal adaptation of the heart from athletics. Fortunately, in most instances, testing can distinguish most patients with HCM from the athletic heart.
What steps can be taken to reduce the likelihood of a problem on the practice field?
Schulman: There is a screening process that can distinguish many, but not all, conditions that could be dangerous to athletic participation. The athlete (or the parent) must be vigilant and report any untoward symptom promptly that could signal a cardiac problem. The symptoms may include untoward weakness, dizziness, loss of consciousness or chest pain around the time of sports participation. A family history of premature death or sudden cardiac death may also be a warning sign.
More information about the sports cardiology program at UConn Health is available at health.uconn.edu/cardiology/clinical-services/sports-cardiology.
Looking at Us: Aretha ‘the Friendly Phlebotomist’ Floyd
If you’ve ever encountered Aretha Floyd, you may have found her so pleasant that you almost could forget she was sticking you with a needle. Aretha is an inpatient phlebotomist who draws blood throughout the University Tower. She’s worked in health care for 23 years, including the last three at UConn Health, where patients and coworkers know her to be friendly, upbeat, and always smiling. Aretha is a mother of five and grandmother of four. She and her husband live in Bristol.

Aretha Floyd
Favorite book:
Are You There God, It’s Me, Margaret by Judy Blume
Favorite time of year:
New Year’s
Favorite place to visit:
Japan
Famous person you’d most like to meet:
Aretha Franklin, because I was named after her!
Something about you today that your younger self would never believe:
I will become a nurse. I’m starting school in January and I’m really excited about it!
What is the most challenging or rewarding aspect of your job?
The most challenging and rewarding thing that I can say that I have here is drawing patients’ blood. Everybody’s scared, they’re nervous, and they’re upset, they don’t know what’s going on with them, and some of them just don’t want to be bothered. But when I come in I just come in with enthusiasm, showing them that I care and that I want them to get their results so they can be well. It’s one of my favorite aspects of things that I need to do to help them get along.
What do most people not know about phlebotomists?
Phlebotomists are nervous too! When we’re drawing their blood, the patient is saying, “Oh my gosh, you’re going to stick me with a needle,” but I’m saying, “Oh my God, I’m going to stick you but I hope I get it on the first try.” Being phlebotomist is a hard job. It’s not as easy as people think it is. When you are really drawing someone’s blood, you have to deal with people from all different races, different thoughts, how they think, you have to try to compromise and have sympathy and empathy for everyone, because everyone doesn’t like needles.
You have a reputation as a very positive and pleasant person. What drives that?
I love my family, friends, and coworkers, and most of all I love people! I love giving respect to people. I don’t care where you come from, who you are, I feel like everyone is my family. I think it’s important that we respect one another, always greet, and say something nice. It doesn’t cost that much. Say something nice.
What would you do to make UConn Health better place?
I would love to have a group of volunteers go into each and every patient’s room and sing. I would love that.
What do you like to do when you’re not at work?
I like to sing with my band, I’m in a five-piece band, we’re called Five Straight. I like to rehearse with them and learn new songs so we can show our talent. We’re not on Facebook yet, but if you need to know where we’re playing, you can come to me, I’ll let you know, I’ll text you, I’ll do whatever I need to do to let you know that we’re playing somewhere.
Spotlight on Services: Day in the Life of a Dispatcher

Our UConn Health dispatchers answer hundreds of calls each day – some of them routine – such as vehicle jumpstarts or door unlocks – others are a matter of life and death. One recent incident called special attention to the great work they do when Buildings and Grounds Patrol Officer Kevin Cabelus kept a distraught, suicidal former patient on the phone talking while dispatcher Stephen Ferraro figured out his identity and location. They contacted local police who rushed to the man’s home and found him clinging to life. Their fast action is credited with saving the man’s life.

The Pulse wanted to learn more about our dispatch services here at UConn Health so we asked Stephen and Kevin to answer a few questions about the important service they provide.
How many dispatchers work at UConn Health?
UConn Health currently has five full-time dispatchers. There are 10 Buildings and Grounds Patrol Officers (BGPO) in the department who are also trained in dispatch to fill in absences on any shift as needed. There is always someone on duty – whether it is a dispatcher or a BGPO – our emergency and routine lines are always monitored by trained staff on campus.
What kind of training does it require?
The full-time dispatchers are sent to the same training course that municipalities send their dispatchers. We also take a course to be certified in COLLECT which is the Connecticut database for accessing everything from driver and license plate information, to stolen cars and wanted or missing persons nationwide. Additionally, dispatchers have specialized training opportunities in active shooter, crisis intervention, self-defense, and radiation. We are also CPR certified.
What types of calls do you receive?
Typical emergencies, such as medical/injury calls, car accidents, thefts, and personnel disputes and routine calls, such as people needing directions or escorts, vandalism, door unlocks, vehicle jumpstarts, wildlife reports, or just anything that people need to know and don’t know who else to ask. Though we strive to help everyone as soon as they call, you may be put on hold for an answer to your routine question when something of an emergency nature is on the other line. We appreciate your patience!
What is the most common call you receive?
This will vary by shift, but because I work at night we do a lot of unlocks in the building and escorts for employees after shuttle service stops. We also have a lot of calls for patients who are disruptive or combative. I send BGPO’s and police officers there to mitigate and isolate these threats and keep staff and the other patients safe and comfortable.
How is it different working here versus a town or city police dispatch?
Basically all the same things that occur in a town can and do occur here on campus at some point. The biggest technical difference is that we do not answer 911. While we have our in-house emergency line, only so many 911 centers are authorized by the state. Since we’re located in Farmington, 911 calls go there initially. If a call is pertaining to our campus, it will be transferred back to us when necessary. In terms of call handling, a big difference is that we are customer service oriented. Whether it’s a call from an employee or one of our many patients and visitors – we are here for everyone, to keep them safe and do what we can to help while they learn, teach, work, heal, grieve, or celebrate life.
Why did you want to become a dispatcher?
Stephen: Being a dispatcher is a great way to help people, which I enjoy being able to do as a career. What led me to this position was a background in volunteer firefighting, giving me experience on the other side of the radio. I had already worked at UConn Health in Nursing Transportation so when this position became available I was very eager to jump at the opportunity to do something I love at a place I’d grown to love as well.
Kevin: I chose public service because I knew at a young age this is what I wanted to do. There are a lot of police officers in my family so it felt natural to get my college degree in criminal justice. Helping people is what I enjoy and there’s no better way to do that than with this career. When you go into any type of law enforcement or public service you build a bond with co-workers that is very strong because you depend on each other every day. For example, the call that Steve and I had, we’ve worked together for a little over 3 years now so when that call came in we knew what the other person needed to make that call successful. When you work with people like Steve and you mesh well together, it makes your shift and career a lot easier.
Any calls that really stand out for you and the dept.?
Collectively all of our dispatchers do great work handling serious calls, they’ve had accidents, they’ve had casualties, they’ve had people running around with weapons or being aggressive on drugs, they’ve had fires and gas leaks… It’s our job as dispatchers to quickly bring about resolution and minimize the impact these incidents have on those involved and the rest of the important things that go on here at UConn Health. Doing so, alongside our excellent team of firefighters, paramedics, police officers and BGPO’s, has been as much of an honor as it has been working with the other dispatchers here at UConn Health.
Healthcare Doesn’t Take a Holiday

When the 26-year old man arrived at our emergency department he was suffering from an excruciating headache. A brain scan found the bad news, a lesion the size of a golf ball. It was causing serious damage and needed to be removed ASAP. But the next day was July 4th – a time for parades, picnics, and fireworks.
“We have limited staffing on the holiday but we all got together and said we’re going to do it, we’re going to get it done,” says Ellen Benson, OR nurse manager. “It doesn’t matter what day of the week it is. Health problems don’t take a holiday.”
The surgery was a complex, requiring special high-tech equipment and extra hands to support changing the position of the patient during the procedure. Along with the primary surgical team, the OR also had a back-up team ready in case another emergency procedure came in that day.
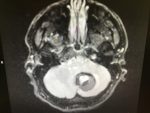
The procedure lasted from 8 a.m. to 3:30 p.m. and went off without a hitch. The patient had a great outcome and is recovering well.
“We continue to demonstrate that the OR team can step up to the plate and deliver the best care possible, no matter what time of day or night it is,” says Benson.
Along with Benson, the team included Agnieszka Korycki, ST; Cathy Spisak, RN; Marissa Knight, RN; Dale Keckley, PA-C; Marc Paradis, MD; Marek Pilecki, APRN; Misha Frenkle; and Ketan Bulsara, MD.
Staff who worked the day before the procedure also played a vital role. “They made sure we had everything that we needed so when we came in all we had to do was execute,” explains Benson. “Lauren Walker, Renee White and Georgia Priestly set us up for success.”
Getting Our Patients to the Portal
 Have you signed up for myHealthONE, our new patient portal, yet? This is a convenient and empowering tool for our patients to manage their health, likely in ways they might not realize, including:
Have you signed up for myHealthONE, our new patient portal, yet? This is a convenient and empowering tool for our patients to manage their health, likely in ways they might not realize, including:
- Viewing test results faster and easier than ever.
- Messaging the office and avoiding telephone hold times.
What better way for our patients to learn about the benefits of myHealthONE than from the providers and staff with whom they come into contact every day? As faculty and staff, the more familiar we are with the portal’s features and advantages, the better equipped we are to share them with our patients. And if you already have signed up, please send your questions and feedback to healthoneupdates@uchc.edu; perhaps you’ll help identify ways to improve myHealthONE and make it more useful for everyone. When our patients use myHealthONE, we all win!
https://www.youtube.com/watch?v=3k2GQrXwJvA&list=PL6h0A_5kXIiR2BrSFC2uz1R5kGdavO_mx
This was first reported in the June 14 Pulse. Watch for additional HealthONE updates in Lifeline, in the Pulse, at uconnhealthexpress.uchc.edu/HealthONE, and on Twitter @UConnHealthONE.
UConn Health Receives Get With The Guidelines-Stroke Gold Plus Quality Achievement Award
 UConn Health/John Dempsey Hospital has received the American Heart Association/American Stroke Association’s Get With The Guidelines®-Stroke Gold Plus Quality Achievement Award. The award recognizes the hospital’s commitment to ensuring stroke patients receive the most appropriate treatment according to nationally recognized, research-based guidelines based on the latest scientific evidence.
UConn Health/John Dempsey Hospital has received the American Heart Association/American Stroke Association’s Get With The Guidelines®-Stroke Gold Plus Quality Achievement Award. The award recognizes the hospital’s commitment to ensuring stroke patients receive the most appropriate treatment according to nationally recognized, research-based guidelines based on the latest scientific evidence.
UConn Health earned the award by meeting specific quality achievement measures for the diagnosis and treatment of stroke patients at a set level for a designated period. These measures include evaluation of the proper use of medications and other stroke treatments aligned with the most up-to-date, evidence-based guidelines with the goal of speeding recovery and reducing death and disability for stroke patients. Before discharge, patients should also receive education on managing their health, get a follow-up visit scheduled, as well as other care transition interventions.
“UConn Health is dedicated to improving the quality of care for our stroke patients by implementing the American Heart Association’s Get With The Guidelines-Stroke initiative,” said Dr. Sanjay Mittal, director of the stroke program. “The tools and resources provided help us track and measure our success in meeting evidenced-based clinical guidelines developed to improve patient outcomes.”
UConn Health additionally received the association’s Target: StrokeSM Honor Roll Elite award. To qualify for this recognition, hospitals must meet quality measures developed to reduce the time between the patient’s arrival at the hospital and treatment with the clot-buster tissue plasminogen activator, or tPA, the only drug approved by the U.S. Food and Drug Administration to treat ischemic stroke.
“We are pleased to recognize UConn Health for their commitment to stroke care,” said Eric E. Smith, M.D., national chairman of the Get With The Guidelines Steering Committee and an associate professor of neurology at the University of Calgary in Alberta, Canada. “Research has shown that hospitals adhering to clinical measures through the Get With The Guidelines quality improvement initiative can often see fewer readmissions and lower mortality rates.”
According to the American Heart Association/American Stroke Association, stroke is the No. 5 cause of death and a leading cause of adult disability in the United States. On average, someone in the U.S. suffers a stroke every 40 seconds and nearly 795,000 people suffer a new or recurrent stroke each year.



