
It’s natural that campus safety, while always a priority, would be even more top of mind following a mass shooting like what took place in Parkland, Florida, last month.
Within the last two years, UConn has shifted to a progressive model, folding police, fire, emergency management, communications centers, and the fire marshal’s office into a single Division of Public Safety. The resources span all campuses, including UConn Health.
Division Director Hans Rhynhart, who is also chief of the UConn Police Department, says the key to readiness for an active threat situation on any campus is preparation and prevention.
“We’ve accomplished and standardized combined training with all division personnel, with police, fire, communications and emergency management, to understand roles and responsibilities to enhance our unified response,” Rhynhart says. “We have threat assessment teams in place which are on the leading edge of trying to prevent a tragedy from happening.”
Part of that prevention component is intelligence gathering. UConn Police have a detective assigned to an FBI Joint Terrorism Task Force, which provides direct access to real-time information on a threat or activity of interest.
“There is almost no better resource than the task force that we have to call upon should we need enhanced, immediate intelligence gathering,” Rhynhart says.
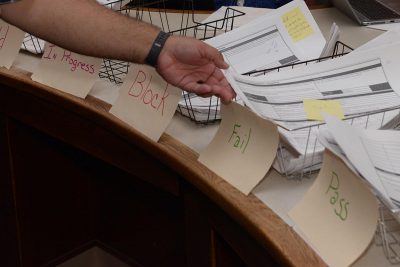
Another Detective works with the U.S. Attorney’s Office on cyber crimes. Social media monitoring is also one of the tools police use to stay aware and gather intelligence. Monitoring can be done on a specific incident or event as well as through the creation of a geo fence to alert investigators to certain phrases and words being used, all with the goal of intercepting and preventing a critical incident from occurring.
Meantime, a general sense of awareness and vigilance in the community can also help with prevention.
“There exists a ‘see something, say something’ philosophy,” Rhynhart says. “If you think that there’s something ‘off’, if you think that an employee or student is acting in a way that is concerning to you, let one of the police officers assigned to your campus know as soon as you can, so we may work with our partners at the University to try to understand what is going on. Most reports we receive are not threatening in nature and do not rise to the level of a criminal violation, but the information gives us an opportunity to talk with and most of the time develop a solution or positive path for an individual. We want to assist in creating a positive and safe environment for all involved.”
An additional component to campus safety is an extensive network of surveillance cameras and blue emergency phones.
The UConn Division of Public Safety offers resources for the public to take an active role in its own safety on its Office of Emergency Management and Community Outreach Unit websites.
“Part of it is being familiar with the information that we put out,” Rhynhart says. “Accessing these websites provides a wide array of tools that will aid in not only your own personal response to hazards, but what you can expect from the University as well. There are fliers and guides, including a campaign we started called ‘Seconds for Safety.’ We break information out into different types of incidents. They’re very quick to consume, you can look at it in seconds, and understand what you should do at any specific moment to ensure a better chance of survival.”



 Debbie Baril
Debbie Baril




 Favorite musician:
Favorite musician:
