Pulse
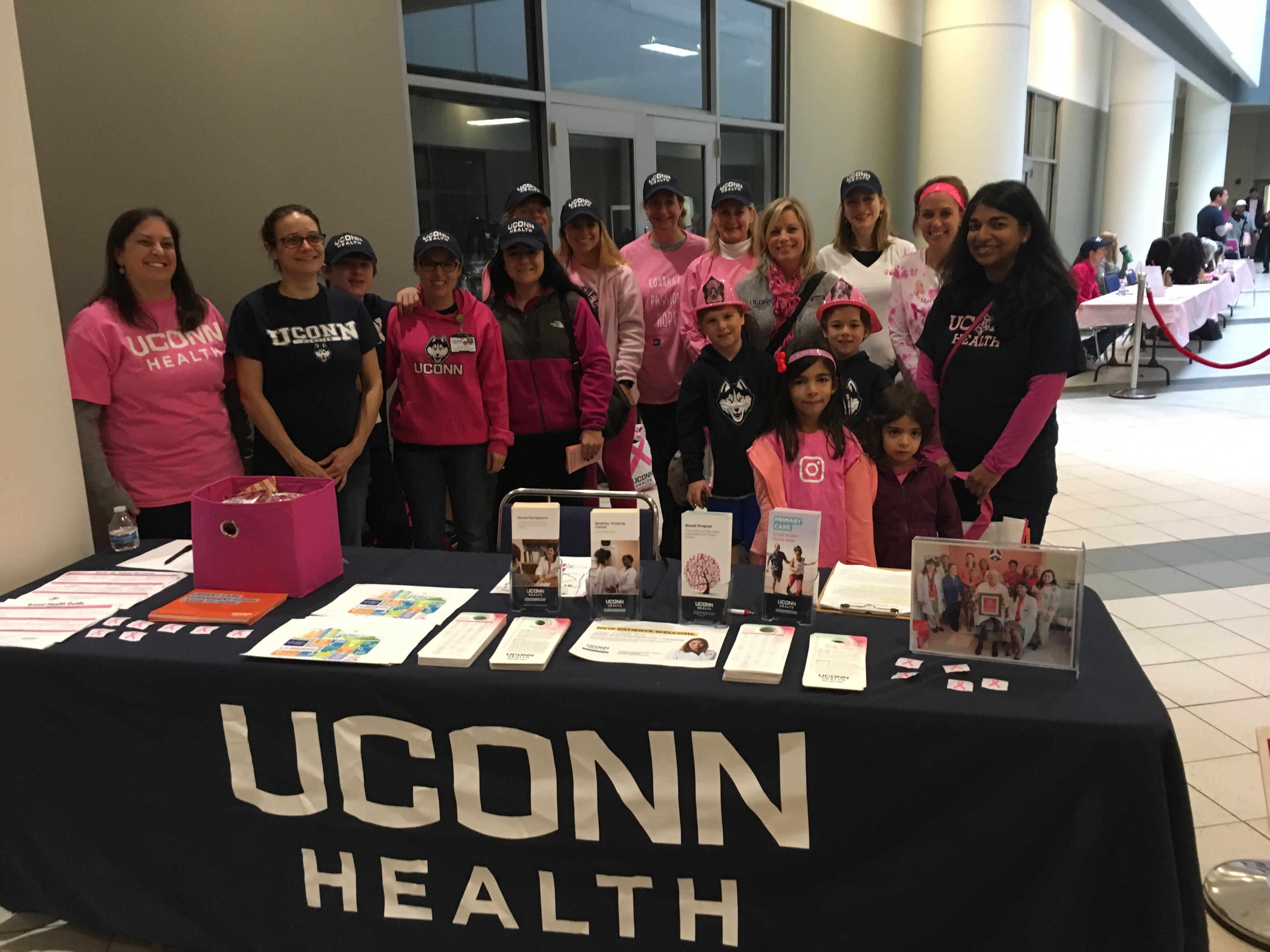
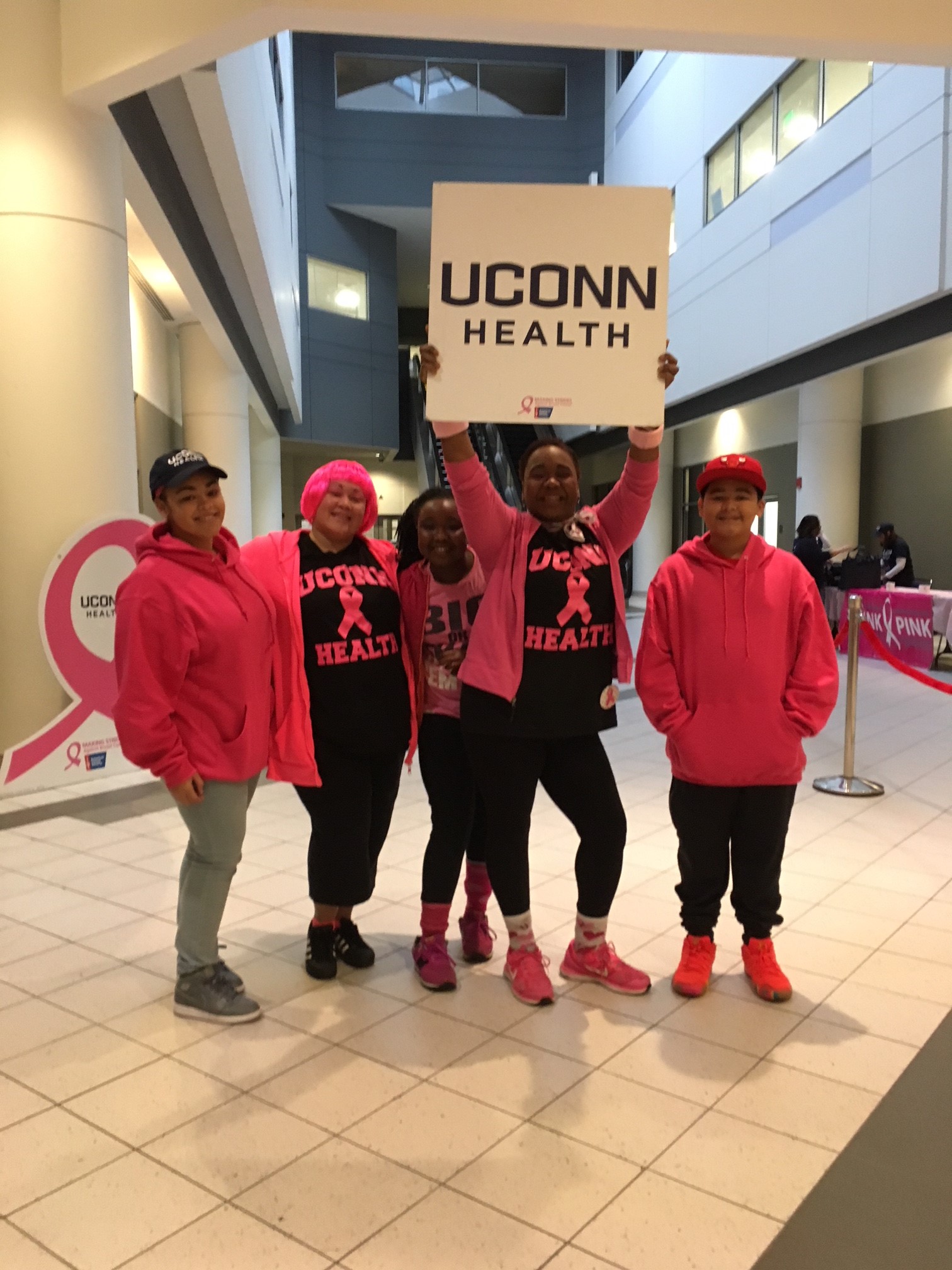
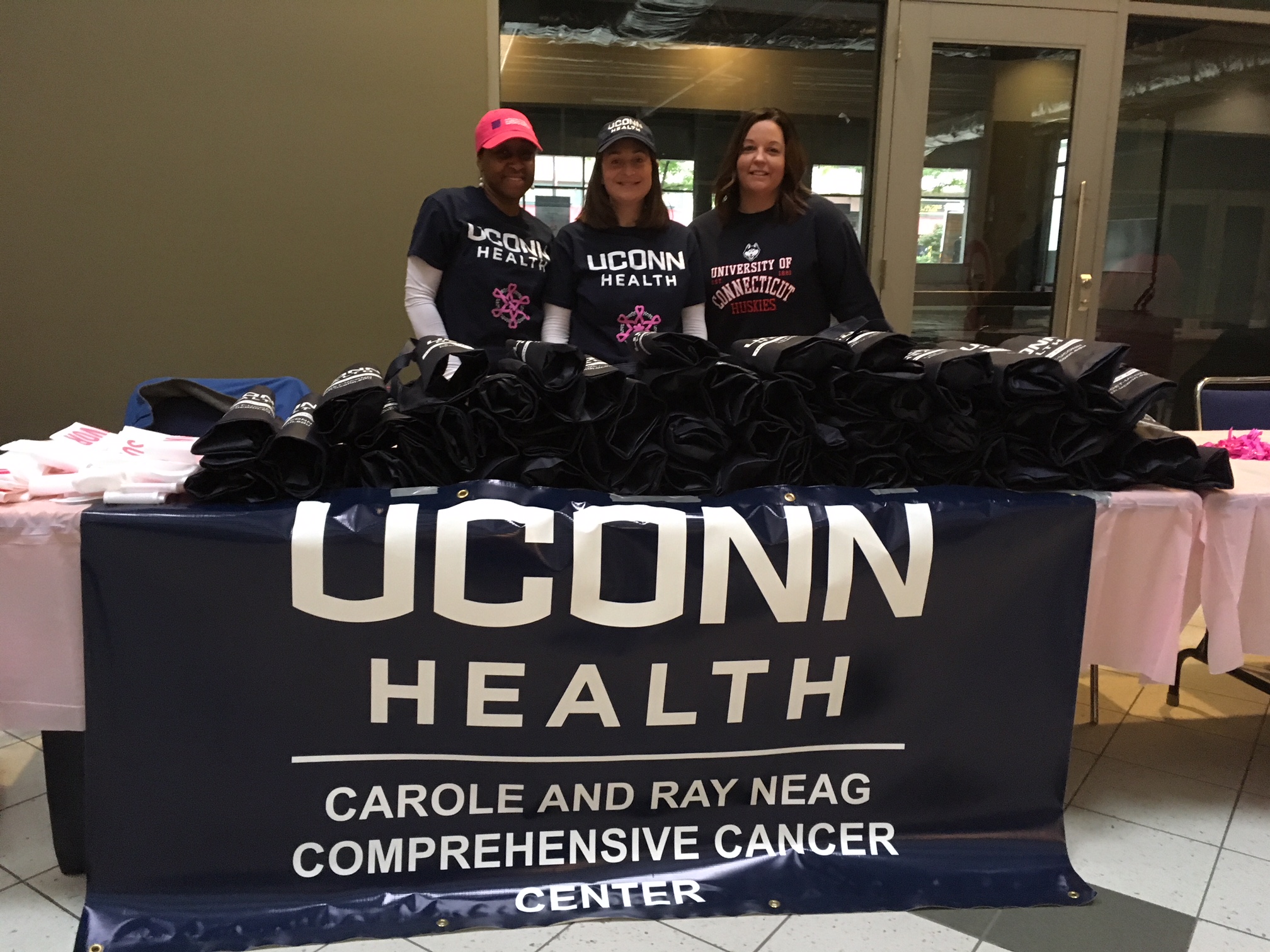
Making Strides 2018
Honoring 25-plus Years of Service
UConn Health hosted a dinner on Wednesday night, honoring employees who have given 25 years or more of service. Dr. Alan Lurie, chair of the Division of Oral and Maxillofacial Diagnostic Sciences was the guest of honor, having served for 45 years. (Photos by Alexis Crean)
Spotlight on Services: UConn NeuroSport

Whether an athlete suffers a traumatic brain injury (TBI) or a persistent neurologic condition, he or she can turn to UConn NeuroSport for diagnosis, treatment, and rehabilitation. Located in downtown Storrs and part of UConn Health Orthopedics and Sports Medicine, NeuroSport enlists multiple specialties to deliver personalized care. Dr. Anthony Alessi, a neurologist who specializes in sports medicine and neuromuscular disease, is the director of UConn NeuroSport.

What kinds of conditions do you see at UConn NeuroSport?
Although everyone is focused so much on concussion and head injuries, and rightfully so, we also take care of athletes with other neurologic injuries, like migraine headaches, epilepsy, and multiple sclerosis. We’re not limited to high-velocity contact sports. Other athletes – runners, non-contact sports athletes, any of those who they feel have a neurologic problem, whether it be acute or chronic – we’re happy to see, even if it’s just to give them a second opinion. Or people who are getting symptoms, as they’re running they’re starting to develop neurologic symptoms, we’re happy to see them.
Who are your candidates for care?
We see all ages, including high school and younger, from throughout the region, including other states. We have elite athletes who fly in and stay at the hotel out here, at the Nathan Hale Inn, and will stay for several days. We put them through the regime based on what we see and who they’re going to see next in the same day. If we need imaging we get that done quickly – we’re now able to do MRI imaging here. We have everything right here in Storrs, including athletic fields to assess athletes on. It’s exciting because it’s growing pretty fast.
What is UConn NeuroSport’s approach to care?
We are familiar with what medications need to be used that are legal, from the standpoint of performance-enhancing drugs, and we have to modify our treatment based on their performance. Some drugs that we would use typically for, say, migraine or epilepsy, will impair performance. Some will cause patients to gain weight, some to lose weight.
We look at all the neurological aspects of sport. When someone comes here with head injury, we typically look at that, verify the diagnosis, and then try to implement a program of getting them back to their sport, working with athletic trainers. It’s a multidisciplinary approach to getting an athlete back. It’s crucial to all of sports medicine, and neurology is no different. UConn, here in Storrs, is one of the few places where we do that through the Department of Orthopedics and Sports Medicine. We’re a growing of group of subspecialists within neurology who do sports.
Which other specialties are involved?
We work with primary care sports medicine specialists, orthopedic surgeons, physical therapists, and athletic trainers.
Who refers patients to UConn NeuroSport?
We get most of our referrals from athletic trainers. When you’re an athletic trainer for a team, your job is to get that athlete back as quickly and safely as you can. Those are the people who are closest to the action.
Second to them are primary care physicians, who evaluate their patients and then send them to us when appropriate. Anytime a physician is faced with a patient who they’re not able to get back in a timely fashion, or they keep meeting obstacles with, those are the people we want to see.
We have athletes with neurologic conditions who compete at the highest level of sport. Who would even imagine that someone could be playing at the highest level of their competitive sport with a diagnosis of multiple sclerosis? But that is going on.
More information about UConn NeuroSport is available at health.uconn.edu/orthopedics-sports-medicine/specialties/neurosport.
Spotlight on Services: Diabetes Education

Diabetes educators are an essential part of the care team for people with diabetes. The UConn Health Diabetes Education Program includes nurses and dietitians – some of whom are certified as diabetes educators (CDE) – as well as physicians, nurse practitioners, physician assistants, exercise specialists, social workers, and other health care professionals. All work together to ensure the best care and management of diabetes.

Jean Kostak is a diabetes education specialist and the program’s coordinator.
How do CDEs fit into the larger care picture?
CDEs are health professionals who work with providers to support patients’ day-to-day efforts managing their diabetes. We can be registered nurses, registered dietitians like myself, pharmacists, exercise specialists or social workers. We take the time to get to know the patients, help them develop a plan, and give them to the tools to take control of their diabetes. Part of that is, as our name suggests, educating patients about their type of diabetes and how it progresses through their lifetime.
What’s the most common question you get?
“What can I eat?” We probably get that the most. We work with patients to individualize their meal plan to help them meet their blood sugar goals and lose weight if needed. Often times they can still enjoy their favorite foods, in reasonable moderation. If you think about it, it’s really not that different than those don’t have diabetes, because really we all should be careful about what – and how much – we eat.


How do you help with the self-management of diabetes?
Good lifestyle choices go a long way in managing diabetes, and the cases of people who have prediabetes, good lifestyle choices can slow down or even prevent progression to type 2 diabetes. This includes of course exercise. We work with patients to teach them how to fit physical activity and exercise into their daily routine regardless of their restrictions. We educate them about their medication and how to take it correctly. And we can assist with choosing the right blood glucose testing monitor and show them how to use it and interpret the results.
Why is this an effective care model?

Managing diabetes can be stressful. Adding to that stress is, if not managed properly, diabetes can lead to other complications. When you have someone to work closely with as you face these challenges, you can build confidence in you ability to self-manage you diabetes. And that can help you feel your best. We have an ongoing relationship with our patients. They don’t have to go through it alone, which can make a big difference in not letting their diabetes get in the way of leading a full, healthy life.
What are the qualifications of a certified diabetes educator?
We must prove our knowledge and skill in diabetes self-management education by completing at least 1,000 hours of patient education and pass a challenging certification exam. Patients can be sure that when they’re working with someone with CDE credentials, they’re in good hands.
November is Diabetes Awareness Month, and this year, National Diabetes Education Week is Nov. 4-10.
Learn more about diabetes care at UConn Health at health.uconn.edu/diabetes.
Keep Calm and Get Your Mammogram
Your co-workers throughout the UConn Health community ask you to join them in raising breast cancer awareness by wearing pink on Friday. Shout out to the UConn Health Internal Medicine sites in East and West Hartford for participating in the cancer center’s Community Breast Navigation Program this year! With their help and expertise, the grant funded outreach program was able to educate women on the importance of screening and provide seamless navigation to screening.
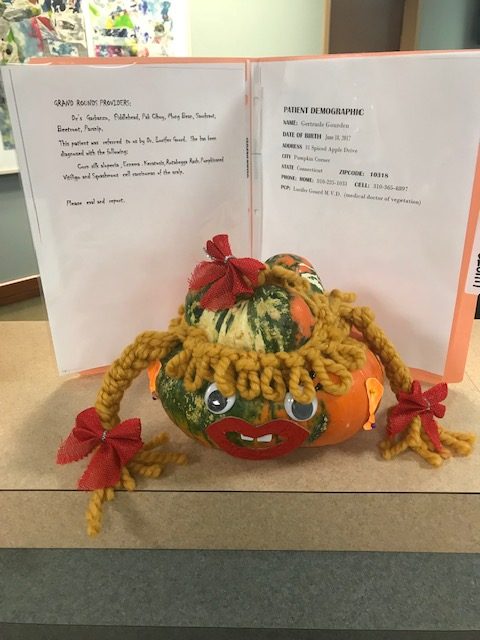
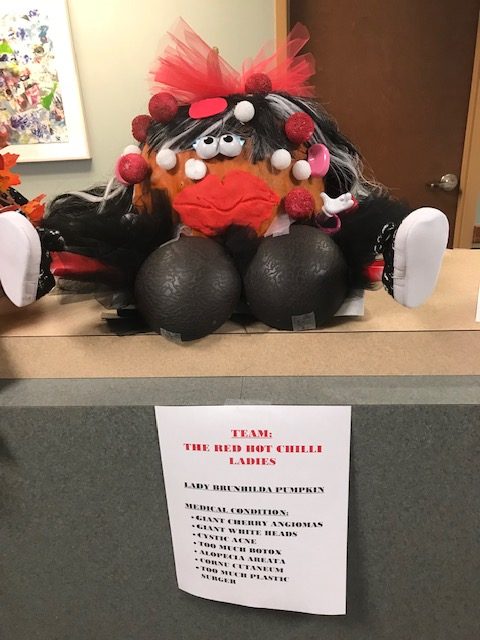
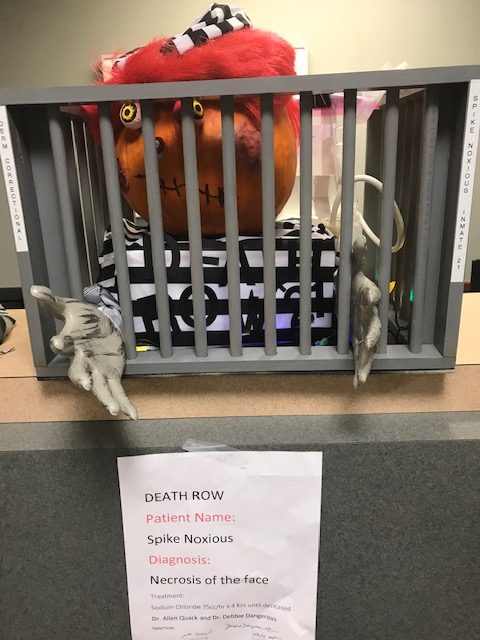
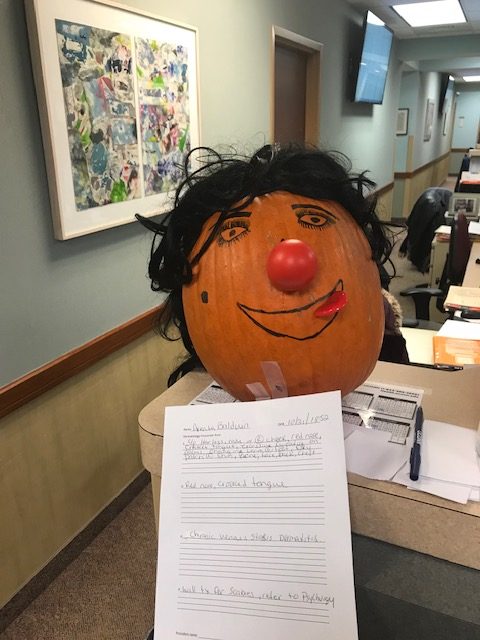
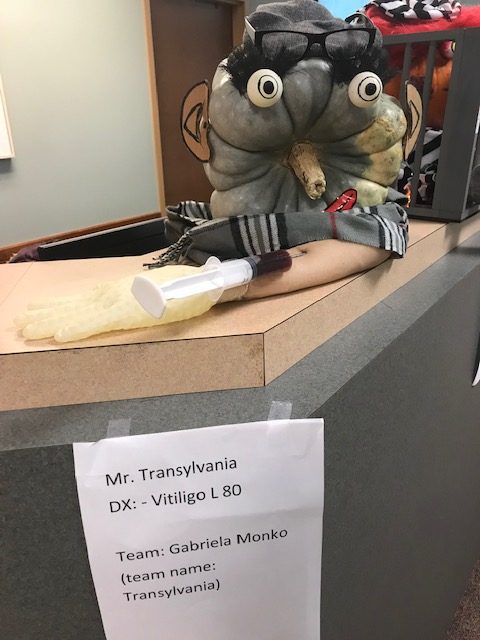
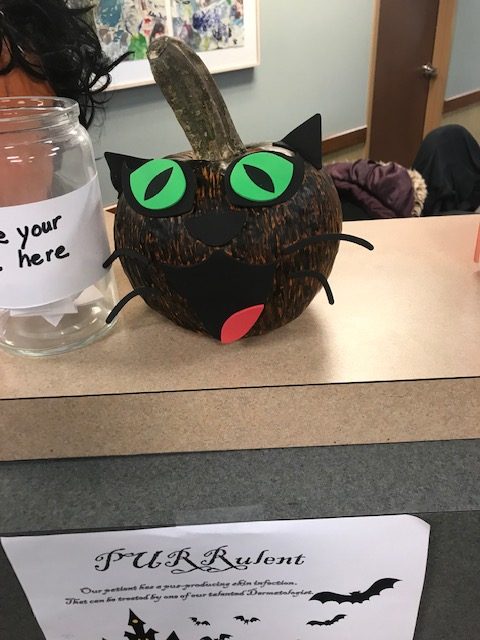
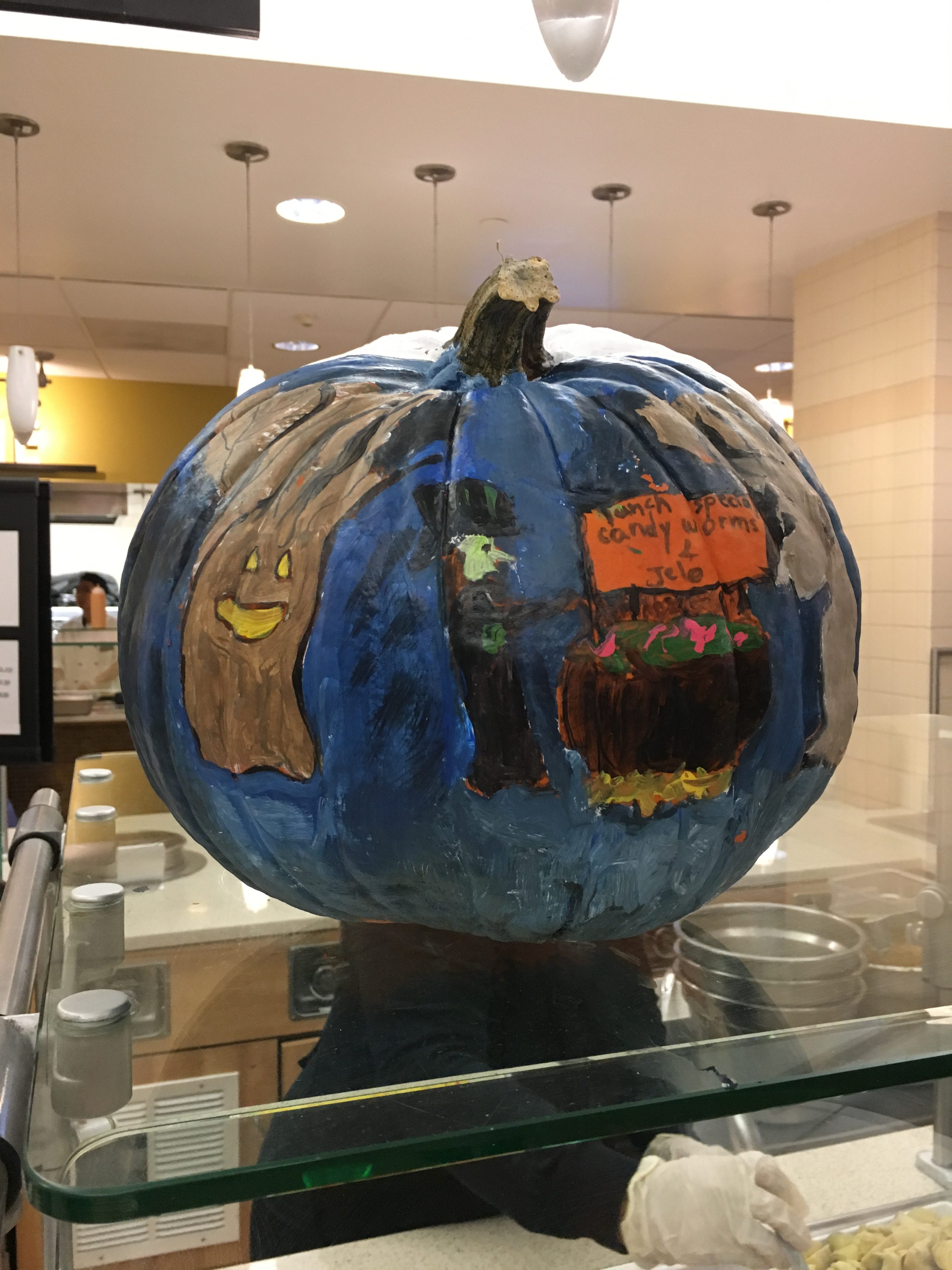
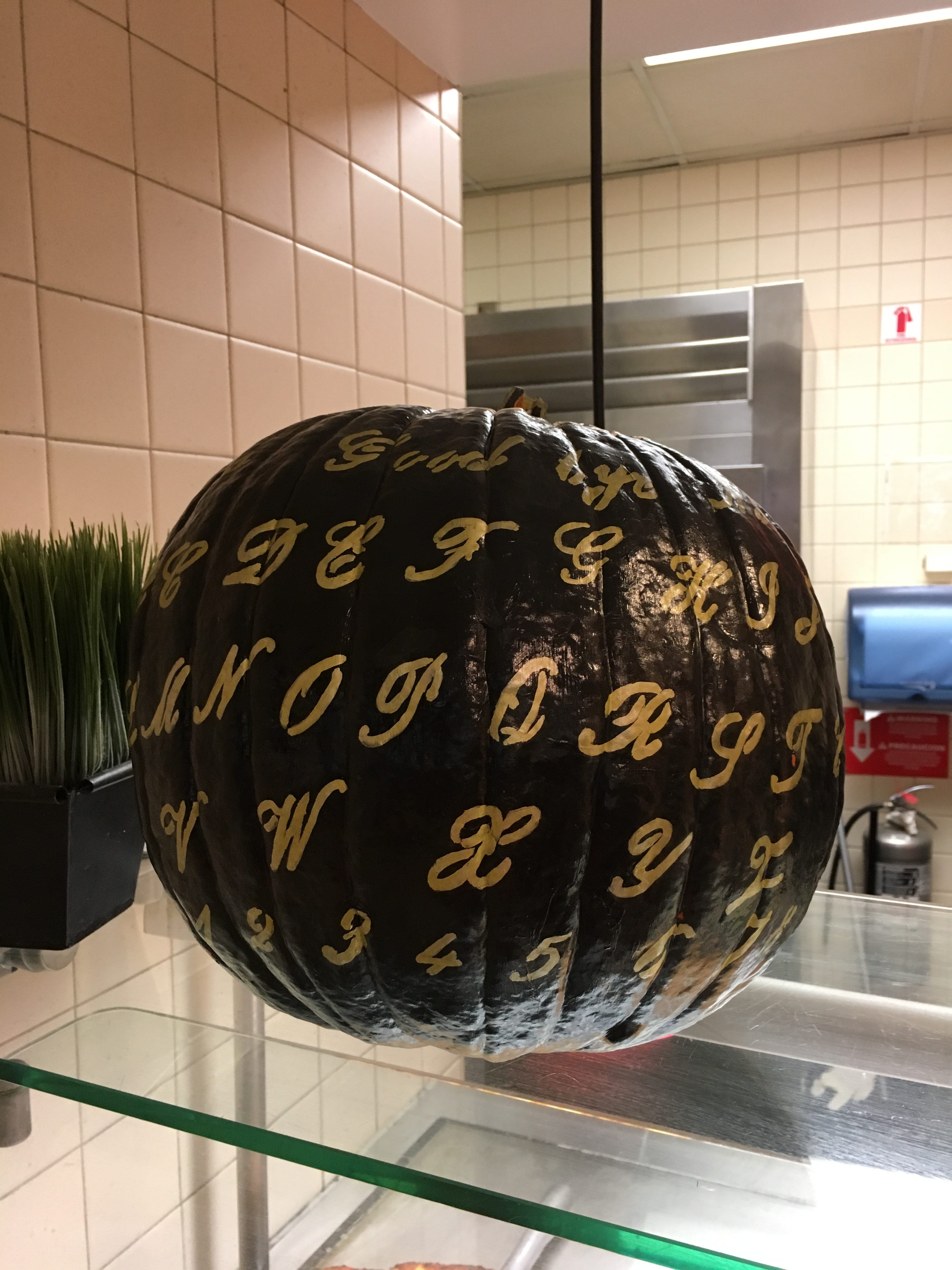
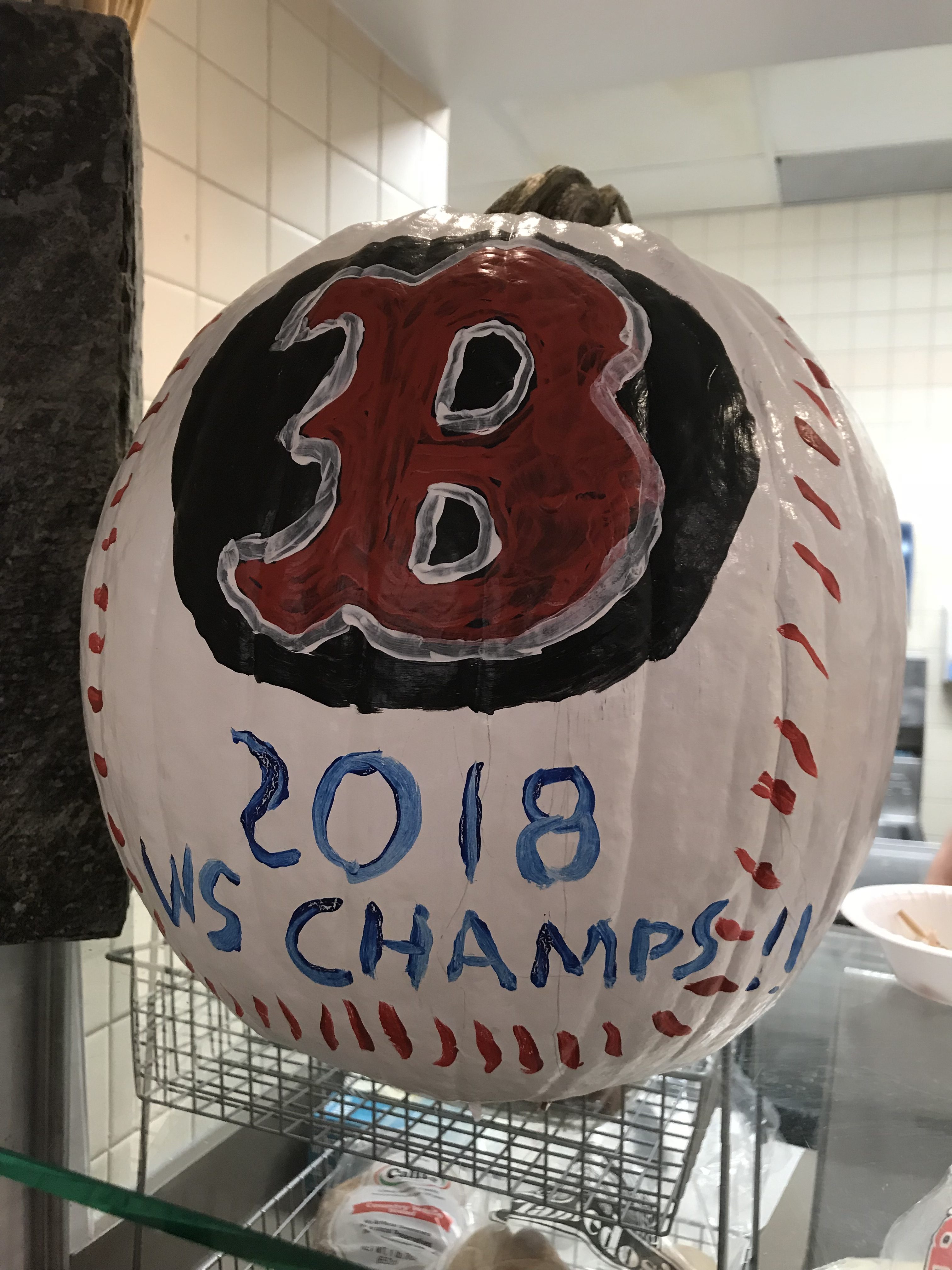
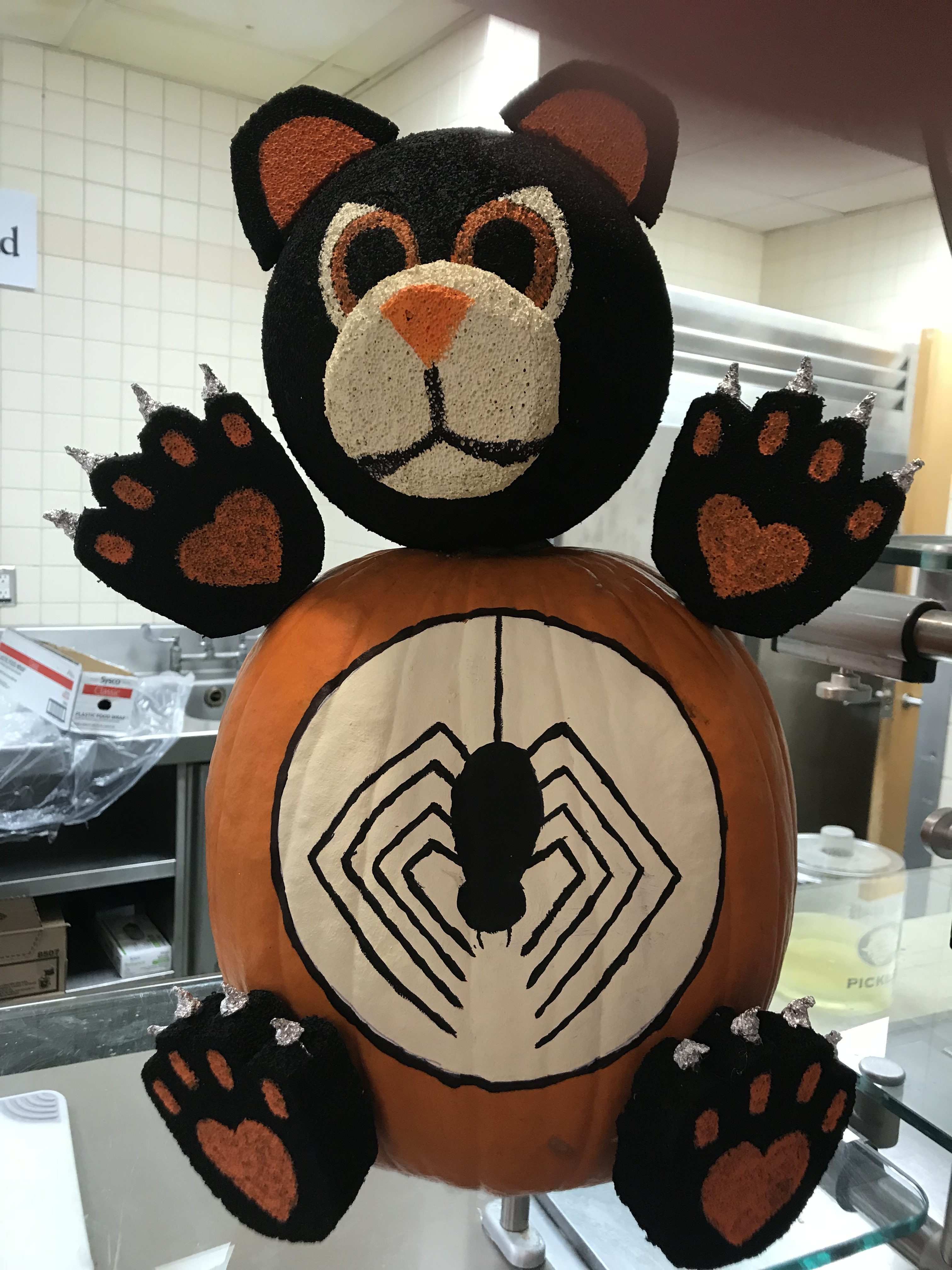
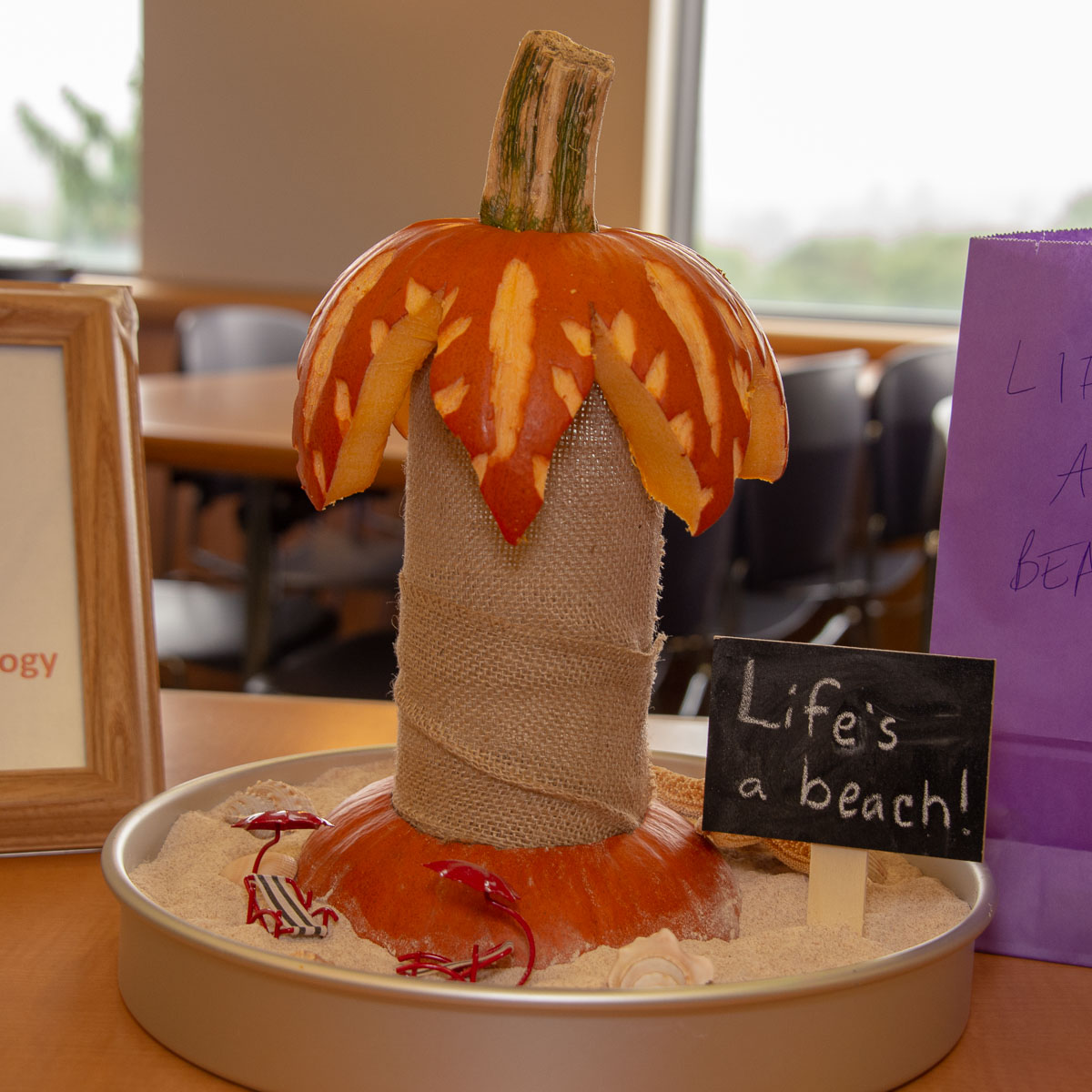
Fall Festival and Pumpkin Palooza 2018
Wet weather didn’t dampen the spirits of all who attended this year’s Fall Festival. More than 1,000 enjoyed the annual autumnal treats and voting for their favorite Pumpkin Palooza entry. Thanks to those who volunteered and quickly turned the cafeteria into a delightful venue for this fall favorite. Photos by Tina Encarnacion.
Looking at Us: Ellen ‘Bleeds Blue’ Benson, OR Nurse Manager
More than 11,000 surgeries are performed here every year from foot surgery to brain surgery which takes a lot of coordination and planning to make sure patients get the best care possible. A key reason our ORs run smoothly and efficiently is the dedication and tireless work of nurse manager Ellen Benson. She’s worked at UConn Health for the last 28 years. Ellen lives in Harwinton with her husband of 36 years. She has three grown children.
 Ellen Benson
Ellen Benson
Favorite book:
I was never much of a reader, but I fell in love with Edgar Allan Poe when I was a kid, weird little short stories, they were great for my attention span at the time
Favorite movie:
I love Harry Potter and Indiana Jones movies.
Favorite time of year:
I love the fall. The cool crisp air, the colors, the smells and the comfort foods (like apple crisp and ice cream). Halloween is one of my favorite “holidays.”
Favorite place to visit:
This is a toss- up. I love the beach and I also love to hike in the woods, no particular location. As long as my family is with me, I’m happy anywhere.
Famous person you’d most like to meet:
Colin Powell. I read his autobiography and was amazed at his life story, the places he has traveled, the work he did, the people that he knew. I would also have loved to have met and worked with Florence Nightingale – she is my hero!
Something about you today that your younger self would never believe:
That I would love my job even more today than I did when I first started and that I would be the manager of the OR.
Why did you become a nurse?
I went to a career fair when I was 18 years old and was introduced to the surgical technology profession. I grew up butchering chickens with my grandfather, so I thought – I can do that job! I worked for about a year full time and then realized I could do more, so my husband encouraged me to go to nursing school.
How did you end up being the OR nurse manager?
I worked for nearly 19 years from 3 to 11 p.m. as a staff nurse. That was an extraordinary opportunity because I learned so much. I worked with a small group who really helped each other and it was an awesome environment. Working evenings also gave me the opportunity to be home during the day with my children. It was the perfect work/life balance for us. When my youngest daughter was in high school, my husband said it was time to switch shifts. It just so happened that the assistant nurse manager position opened up. I had never thought about going into management but I thought that it might be a good move for me. I got the position and learned many new skills. When the manager position became available, a few people encouraged me to apply. Much to my surprise, I was hired for the position and have been the manager for almost five years now.
What has been a major milestone in your career?
I earned my bachelor’s degree about a year ago. That was a huge personal achievement! I was highly encouraged to complete my degree by nursing administration and they really supported me through the process. I enjoyed taking classes with the younger students who were fresh out of their associate degree programs. I have worked in the OR my whole life so it was great looking at nursing through their eyes. I ended up being a mentor to quite a few of them and I still stay in touch with them, so that was really a wonderful experience. My husband and children also helped me achieve this milestone, if it weren’t for their support, it would have never happened.
Why do you like working at UConn Health?
It’s just a wonderful place to work. We have this beautiful new hospital and we have great nurses, physicians and support staff to help us fulfill our mission of teaching and caring for the people of the state of Connecticut.
I love coming to work every day. I am proud to be a part of the UConn family.
I really do bleed blue!
Faculty Appointments and Promotions Fall 2018
The Academic Affairs Subcommittee of the Board of Directors during its September meeting approved the following School of Medicine and Dental Medicine faculty promotions and appointments:
School of Dental Medicine Promotions
Professor (Continuing Tenure)
Dr. Efthimia Ioannidou, Division of Periodontology
Dr. Rajesh Lalla, Division of Oral and Maxillofacial Diagnostic Sciences
Professor (In-Residence)
Dr. Yu-Hsiung Wang, Division of Pediatric Dentistry
Associate Professor (In-Residence)
Dr. Bina Katechia, Division of Pediatric Dentistry
School of Medicine Appointments
Professor – Affiliated
Dr. Mark D. Adams – (The Jackson Laboratory) – Genetics and Developmental Biology
Dr. Mark J. Alberts – (Hartford Hospital) – Neurology
Dr. Glenn Flores – (Connecticut Children’s Medical Center) – Pediatrics
Dr. Daniel Grow – (Center for Advanced Reproductive Services) – Obstetrics and Gynecology
Associate Professor – Tenure Track
Dr. William S. Shaw – Medicine
Associate Professor – Affiliated
Dr. Beth C. Natt – (Connecticut Children’s Medical Center)
School of Medicine Promotions
Professor – with Award of Academic Tenure
Dr. Royce Mohan – Neuroscience
Professor – In-Residence
Dr. Qian Wu – Pathology and Laboratory Medicine
Professor – Affiliated Institution
Dr. Karan M. Emerick – (Connecticut Children’s Medical Center) – Pediatrics
Clinical Professor – Community Faculty
Dr. Anthony G. Alessi – Neurology
Award of Academic Tenure
Dr. Annabelle Rodriguez-Oquendo – Cell Biology
Associate Professor – In-Residence
Dr. David B. Banach – Medicine
Dr. Stacey L. Brown – Community Medicine and Health Care
Dr. Ramaswamy M. Chidambaram – Genetics and Genome Sciences
Dr. Jessica M. Clement – Medicine
Dr. Thomas J. Devers – Medicine
Dr. Katalin Ferenczi – Dermatology
Dr. Alise Frallicciardi – Emergency Medicine
Dr. Karen M. Hook – Medicine
Dr. Juyong Lee – Medicine
Dr. Faryal S. Mirza – Medicine
Dr. Karen L. Steinberg – Psychiatry
Dr. Haleh Vaziri – Medicine
Dr. Siu-Pok Yee – Cell Biology
Associate Professor – with Award of Academic Tenure
Dr. Dmitry M. Korzhnev – Molecular Biology and Biophysics
Dr. Yi I. Wu – Genetics and Genome Sciences
Associate Professor – Affiliated Institution
Dr. Thyde Dumont-Mathieu – (Connecticut Children’s Medical Center) – Pediatrics
Dr. Alex B. Golden – (Connecticut Children’s Medical Center) – Pediatrics
Dr. Katherine R. Kavanagh – (Connecticut Children’s Medical Center) – Surgery
Dr. Kristan A. Pierz – (Connecticut Children’s Medical Center) – Orthopaedic Surgery
Dr. Wael N. Sayej – (Connecticut Children’s Medical Center) – Pediatrics
Dr. Adam M. Silverman – (Connecticut Children’s Medical Center) – Pediatrics
Dr. Christine M. Skurkis – (Connecticut Children’s Medical Center) – Pediatrics
Dr. Michael J. Soltis – (Connecticut Children’s Medical Center) – Pediatrics
Dr. Adam C. Steinberg – (Hartford Hospital) – Obstetrics and Gynecology
Associate Clinical Professor – Community Faculty
Dr. Seth M. Brown – Surgery
Dr. Jeffry L. Nestler – Medicine
Dr. Belachew Tessema – Surgery
Spotlight on Services: Sports Cardiology

Sports cardiology is an emerging subspecialty with a focus on highly active people. It’s now available at the Pat and Jim Calhoun Cardiology Center, where Drs. Kai Chen and Peter Schulman are among those trained in this discipline, supporting not only UConn athletics but also the Connecticut Sun professional women’s basketball team and the New England Black Wolves professional lacrosse team.
What is sports cardiology?
Chen: Sports cardiology is cardiology related to sports and exercise, an entity incorporating all ages, from childhood to the senior population, and all forms of exercise activity, including professional, recreational, and occupational. Starting with the care of competitive athletes, sports cardiology has expanded to include the general population in the prevention and management of cardiac conditions during exercise.
Who is a candidate to see a sports cardiologist?
Chen: Sports cardiology takes care of athletes and anyone who exercises. Candidates for a sports cardiology evaluation include:
- Healthy people with a family history of cardiac condition before participation in sports or exercise.
- Anyone with new symptoms during exercise or sports participation such as lightheadedness, palpitation, shortness of breath, chest discomfort, or unexplained drop in exercise tolerance.
- Patients with known cardiovascular disease who want to return to exercise and stay active.
How does this discipline fit in with the service as team physicians to the UConn athletic programs?
Schulman: UConn Health physicians serve as the team physicians for UConn athletes, and this is part of sports cardiology. For example, we screen the UConn athletes as they prepare for the upcoming season. Sports injuries and other medical conditions are handled by the UConn infirmary and UConn Health providers in Storrs. Between these two services, UConn athletes have all of their health needs served.
What’s the difference between athletic heart syndrome and hypertrophic cardiomyopathy?

Schulman: Due to increased metabolic demands of athletic performance, the athlete’s heart adapts to the enhanced metabolic needs by undergoing structural changes to increase the ability of the heart to pump blood. These changes include “bulking up” or hypertrophy of the heart muscle and increasing the size of the heart chambers to handle the increased blood flow. These changes are part of the “athletic heart syndrome.” On the other hand, there are some diseases of the heart muscle such as hypertrophic cardiomyopathy (HCM) that can cause adverse structural changes of the heart. HCM can appear superficially similar to the normal adaptation of the heart from athletics. Fortunately, in most instances, testing can distinguish most patients with HCM from the athletic heart.
What steps can be taken to reduce the likelihood of a problem on the practice field?
Schulman: There is a screening process that can distinguish many, but not all, conditions that could be dangerous to athletic participation. The athlete (or the parent) must be vigilant and report any untoward symptom promptly that could signal a cardiac problem. The symptoms may include untoward weakness, dizziness, loss of consciousness or chest pain around the time of sports participation. A family history of premature death or sudden cardiac death may also be a warning sign.
More information about the sports cardiology program at UConn Health is available at health.uconn.edu/cardiology/clinical-services/sports-cardiology.