This article first appeared in the October issue of “Clinical Effectiveness and Patient Safety Forum,” written by Jennifer Sposito.
UConn Health John Dempsey Hospital’s Primary Stroke Center had strong representation at the 10th annual Northeast Cerebrovascular Consortium (NECC) Summit, which was held Oct. 22-23 in Newport, R.I. The goal of this conference is to improve stroke care in the Northeast, share best-care practices, and highlight regional trends to decrease stroke mortality. Two members of the UConn Health John Dempsey Hospital staff presented at the conference:
Peter Canning, paramedic, R.N., and EMS coordinator, this year’s Invited Emerging Practice Lecturer, spoke to the assembly on “Hospital and EMS Stroke Care Partnership: Data Collection, Education and Feedback.” UConn Health is a pioneer in utilizing EMS data to improve care.
 At UConn Health, every stroke and every stroke alert that comes in from EMS is tracked (even when it turns out not to be a stroke), along with the following data elements:
At UConn Health, every stroke and every stroke alert that comes in from EMS is tracked (even when it turns out not to be a stroke), along with the following data elements:
- Dispatched lights and sirens
- Response within 8 minutes
- ALS care
- Stroke recognized
- Cincinnati Stroke Scale
- Blood glucose
- On scene 15 minutes or less
- Last known well time
- Transported lights and sirens
- Stroke alert
- Stroke Alert direct to CT scan
- TPA
- Ischemic vs. hemorrhagic
- Symptoms for missed strokes
- Diagnosis for false alerts
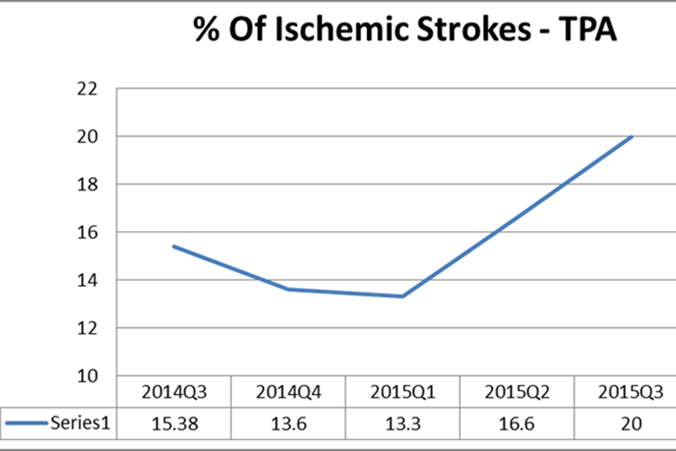
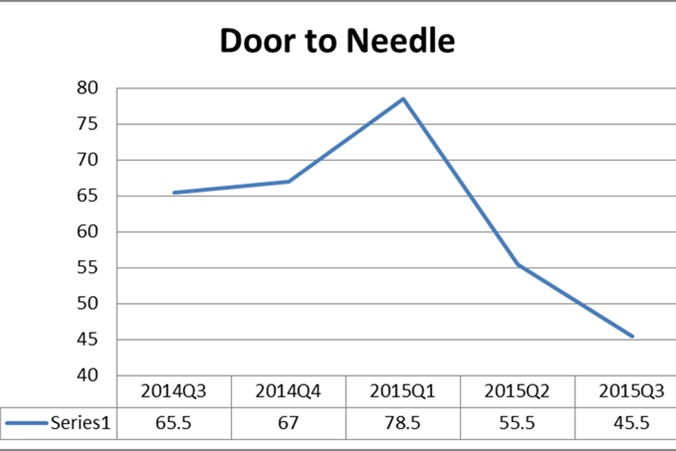
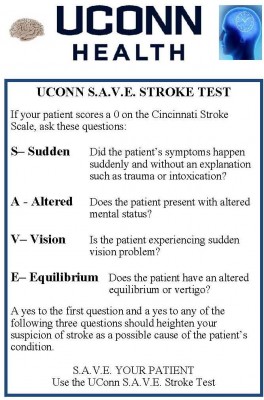
Collecting and analyzing data on EMS response to stroke patients has enabled UConn Health to rewrite pre-hospital stroke care guidelines. Our efforts, which included the development of the UConn S.A.V.E. Stroke Test to increase awareness of the different ways stroke can present, have helped UConn Health lower door-to-needle times and increase the percentage of stroke patients receiving life-saving, clot-busting medicine.
At UConn Health, we consider EMS our partners in stroke care. We recognize that care for our patients truly begins when EMS arrives at their side. Our hospital/EMS partnership works for the benefit of all.
Jennifer Sposito R.N., BSN, stroke coordinator, presented a poster on behalf of UConn Health’s Stroke Center titled: “Measuring Impact of Pharmacist Intervention in Acute Stroke Management by Preparing rTPA in the Emergency Department.” This presentation was made with support from:
- Sanjay Mittal, M.D., Medical Director of the Stroke Program
- Kathleen Coyne, R.N, BSN; Director of Critical Care Nursing
- Allison Dias, Pharm.D., R.Ph.; Medication Safety Pharmacist
- Kimberly Metcalf, M.S., Pharm.D., Director of Pharmacy

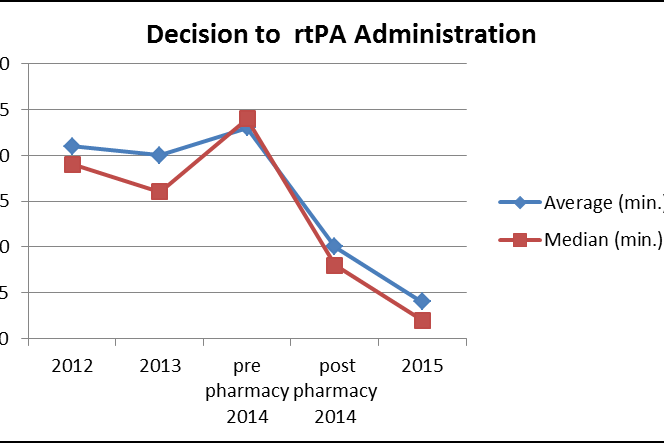
To summarize, a pharmacist responds to the emergency department with a pre-assembled stroke kit, which includes all necessary items and supplies to calculate, prepare, and administer rtPA to an eligible patient. If the patient is an appropriate candidate for rtPA, the pharmacist then calculates the dose and prepares the rtPA for administration, while the emergency department staff prepares the patient for administration of the medication.
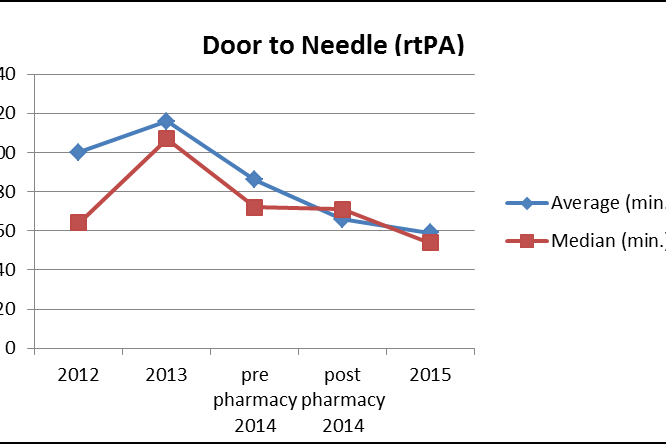
We have seen drastic improvements in the average rTPA order time to rTPA administration as a result of the creation of a Stroke Kit and the addition of a pharmacist to the stroke team. Since implementation of this practice, more than half of our rTPA cases have decision-to-needle times of zero, and we have seen an overall decrease in our average door-to- needle times.
This was a collaborative quality improvement and best practice pilot study that has changed the way we provide optimal care in a timely manner to our stroke patients.
Having a pharmacist present alleviates dosing calculations and preparation of rTPA from emergency department, neurology, and radiology staff and allows each discipline to focus on their clinical duties during a stroke alert. This allows for better collaboration and a reduction in our time to administration, which is imperative to preserve brain function.
A pharmacist utilizing a stroke kit to prepare rTPA directly in the emergency department played a huge part in UConn Health reaching our benchmarks as a primary stroke center.
The unprecedented collaboration among the members of the stroke team, the emergency department staff, and the pharmacy department demonstrates the high quality stroke care we provide at our organization.