
The UConn Migrant Farm Worker Clinics received national media exposure this week after being featured on the Spanish language Univision Network (watch video). The segment was part of a series of reports that aired during Univision’s special Health Week campaign June 6-13.
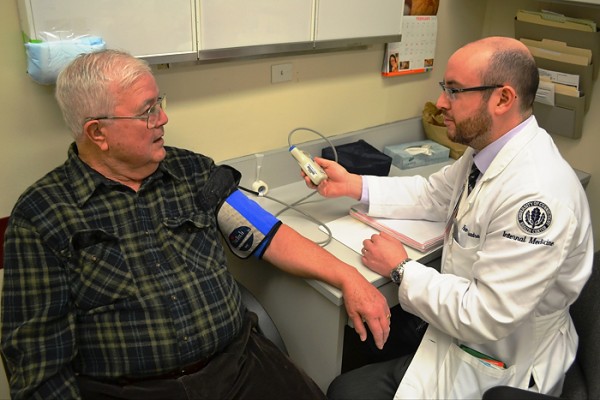
The migrant farm worker clinics are organized and run by health profession students involved with the Connecticut Area Health Education Centers (CT AHEC) Program at UConn Health. The students, along with physician advisors and volunteer interpreters, help provide medical and dental screenings for the hundreds of migrant workers who come to Connecticut each growing season.
The lifesaving care they provide caught the attention of Univision producer Emilce Elgarresta. She contacted Dr. Bruce Gould, UConn Health’s associate dean of primary care who started the mobile health clinics in 1997. Elgarresta said she wanted to do a story about the clinics because she was very impressed and moved with Dr. Gould’s commitment to help the farm workers.
“Migrant farm workers are among the most economically disadvantaged and most medically vulnerable groups in the United States having little, if any, access to health care or medication,” says Gould. “The clinics are a way to provide them much needed medical care while teaching students that caring for the poor and vulnerable is part of the gift of being a health care provider.”

A few weeks later, Elgarresta flew to Connecticut from Miami and she and her crew spent two days in Connecticut taping the story. The segment highlighted the clinic held recently at the Thrall Tobacco Farm in Windsor where workers from Puerto Rico and Mexico took advantage of the free health exams.
Hannah Kotler, a second-year medical student and one of last year’s clinic coordinators, and Dr. Kenia Mansilla, a family medicine physician in Hartford and a longtime clinic volunteer, were interviewed in Spanish for the segment.
The story is part of a yearly campaign by Univision, the fifth largest television network in the U.S., to provide their audience with information about timely health care topics and disease prevention. The stories are aired across the network’s news and entertainment shows, as well as their radio networks, webcasts and town hall broadcasts.
The UConn Migrant Farm Worker Clinics operate annually from June to October and provide services to more than 400 migrant farm workers at nine farms and greenhouses throughout the state. The clinic engages pre-health professions students including high school and college students, as well as health professions trainees and residents.
The Connecticut Area Health Education Center Network (CT AHEC) is a federal and state funded program supporting primary care workforce development. CT AHEC is located within the University of Connecticut’s Center for Public Health and Health Policy at UConn Health in Farmington, Conn.








 for Advanced Certification for Primary Stroke Centers. The Gold Seal of Approval® and the Heart-Check mark represent symbols of quality from their respective organizations.
for Advanced Certification for Primary Stroke Centers. The Gold Seal of Approval® and the Heart-Check mark represent symbols of quality from their respective organizations.
